PRESCRIPTION REQUIREMENTS FOR MEDICAID
Listed below you will find information regarding the following topics:
- When is a Prescription Required for a Medicaid-Related Service?
- What is Required on a Medicaid-Complaint Prescription?
- Verification Process: What Should I be Checking?
- Where Can You Obtain a Medicaid-Compliant Prescription Template?
- Corrections Made to Medicaid Documents
- Electronic Signatures
- Best Practices
- Prescriptions & Billing
------------------------------------------------------------------------------------------------------
1. WHEN IS A PRESCRIPTION REQUIRED FOR A MEDICAID-RELATED SERVICE?
Prescriptions are required for each IEP period as noted below. *
- Annual Review meeting (If the summer session is on a separate IEP from the winter session, a separate prescription is required for each session is required.).
- Whenever a review meeting results in a change in service(frequency/duration/class size); however, a prescription is required only for the service that was changed. The unaffected service(s) do not require a new prescription.
- Child transfers to another school district (transfer meeting).
- New Referrals (newly-identified students).
(* Annual Review/Re-Eval Meeting * Change in Service * Transfer Meeting * New Referral)
* Important Notes:
The “As per IEP” reference to the frequency and duration does not apply once the IEP changes. A new prescription is
required for any of the circumstances listed above.
Medicaid expects a new order/referral:
- At least once a year;
- When the ordered service changes (refer to Q&A 156); and,
- If there is a new IEP. (New IEP usually means an initial IEP or the mandated annual review.)
2. WHAT IS REQUIRED ON A MEDICAID-COMPLIANT PRESCRIPTION(ORDER / RECOMMENDATION)
Per the Medicaid Provider Policy and Billing Handbook (Update 9) on (www.oms.nysed.gov/Medicaid), there are
eight (8) required elements on a written order.
- Child’s Name (Date of Birth is not required, but must be correct if added to the prescription.)
- Term of Service (Specific dates and/or school year dates)
- Service(s) being ordered (OT/PT/ST). (The frequency and duration of the ordered service must be either specified on the order itself or the order can explicitly adopt the frequency and duration of the service in the IEP reference.) (Using the IEP reference is "best practice" and will reduce the chance of potential issues. The Medicaid requirements stipulates that the actual referenceORIEP reference should be used -- not both.)
- Patient diagnosis/need for service(s) (ICD Code)
- Signature of the ordering practitioner (Stamps are not permitted.)
- Date (MM-DD-YR) the order was written and signed
- Ordering Practitioner’s NPI or license number (NPI # 1234567890 / NYS Lic. # 123456)
- Ordering Practitioner’s Contact information (including the address and phone number including area code)
3. VERIFICATION PROCESS: WHAT SHOULD I BE CHECKING?
What makes an uploaded written order invalid?
- Is the handwriting legible for all eight required elements?
- Is any information missing (ltems left blank)?
- If a stamp was used, is it readable or is the stamp covering other pertinent information on the order?
- Is the name and DOB correct?
- Does the order include a term of service (7/1/19 - 6/30/20) or school year (2019-20)?
- Is the frequency/duration delineated on the order (2 x 30) - OR - Is the frequency/duration adopted by explicit reference to the IEP (Frequency/duration as per the 2019-20 IEP)? (It is not recommended to delineate both the actual reference and IEP reference on the order.)
- Are the dates on the order expressed as complete dates? (MM/DD/YR)
- Is there a diagnosis or reason/need for the service on the order?
- Is the order signed (with an original handwritten signature or electronic/digital signature) and dated (with a complete date - MM-DD-YR)?
- Does the order include the practitioner's address and phone number including area code? (If a stamp was used, was it stamped over other pertinent information?)
- During the upload process, an incorrect Medicaid document (Consent form instead of a written order) or a document for a different child is uploaded.
- A document was scanned but is not readable due to lines and dark spots on the image or a document was scanned and some of the information was cut off.
- Were there any corrections made to the order? If so, were they made in accordance with Medicaid relations (*Medicaid Questions and Answers (Question 133) http://www.oms.nysed.gov/medicaid/q_and_a/q_and_a_combined_revised_12_9_16.pdf)?
- A Medicaid-compliant written order verification checklist is available from the Portal Knowledge Base: http://support.cpseportal.com/kb/a173/medicaid-compliant-written-order-checklist.aspx
4. WHERE CAN YOU OBTAIN A MEDICAID-COMPLIANT PRESCRIPTION TEMPLATE?
5. CORRECTIONS MADE TO MEDICAID DOCUMENTS
What is the proper way to make corrections on Medicaid documentation? *
- If a written order needs correction, the ordering provider/practitioner must put a line through the error and initial the change. The corrected information must be visible to an auditor(e.g.,
material to be deleted (TF).
The following is not an acceptable way to correct Medicaid documents:
- White-out or correction tape should never be used.
- Pencil should never be used.
- Documents using these correction methods will be invalidated for Medicaid claiming.
*(Medicaid Questions and Answers (Question 133) http://www.oms.nysed.gov/medicaid/q_and_a/q_and_a_combined_revised_12_9_16.pdf)
6. ELECTRONIC SIGNATURES
Acceptable methods of signing:
- Original hand-written signature
- Signed with a electronic or digital signature*
* (Electronic/digital signatures must have a password or pin # as a method of signing to ensure that only the person authorized can affix the electronic signature. Also there must be a record of who added the signature, when the record was created, that the record cannot be altered or, if altered, records the original and altered versions, dates of creation/creator. If the signature does not include these features, it is not an electronic/digital signature.)
Unacceptable methods of signing:
- Signature stamp
- Scanned "image" of a signature (e.g., JPEG)
- Font substitution for signature (Signature)
7. BEST PRACTICES
- All therapists(OT/PT/SP) should make sure that their written orders are Medicaid-compliant prior to servicing a child. (Use the checklist available from the Portal Knowledge Base -http://support.cpseportal.com/kb/a173/medicaid-compliant-written-order-checklist.aspx)
- Agencies should make sure that all the written orders they receive prior to servicing a child meets all Medicaid requirements prior to servicing a child.
- If the written order does not meet all the Medicaid requirements, a new order should be requested immediately to ensure all services provided comply with the Medicaid regulations.
- Check the document to make sure all eight required items are completed on the Rx template; no blanks. (Also make sure the practitioner's contact information, NPI/License stamps are not placed over other pertinent information on the order.)
- Handwriting should be legible for all eight required items.
- Scanned documents should be checked to ensure that all content was scanned and the image is clear/readable.
- Check the document to ensure that corrections were made in accordance with the Medicaid regulations (white-out, correction tape or pencil are not permitted).
- Make sure you are using the most recent prescription template from the County or you can use the Medicaid-compliant template from the Portal Knowledge Base - http://support.cpseportal.com/kb/a172/medicaid-compliant-prescription-template.aspx.
8. PRESCRIPTIONS & BILLING
For Nassau and Westchester Counties:
- A prescription must be uploaded to the Portal before you can submit billing.
- If you upload a prescription that is later invalidated because it does not meet Medicaid requirements, the status will return to "missing" and you will need to upload a "valid" prescription in order to submit billing.
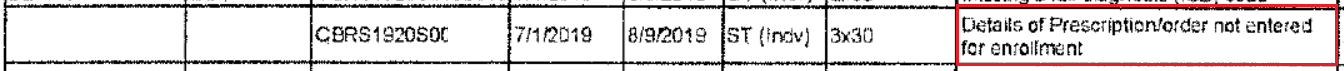
- Listed below is an example of the error message you will see when a valid prescription is not uploaded to the Portal when you submit billing.